Description
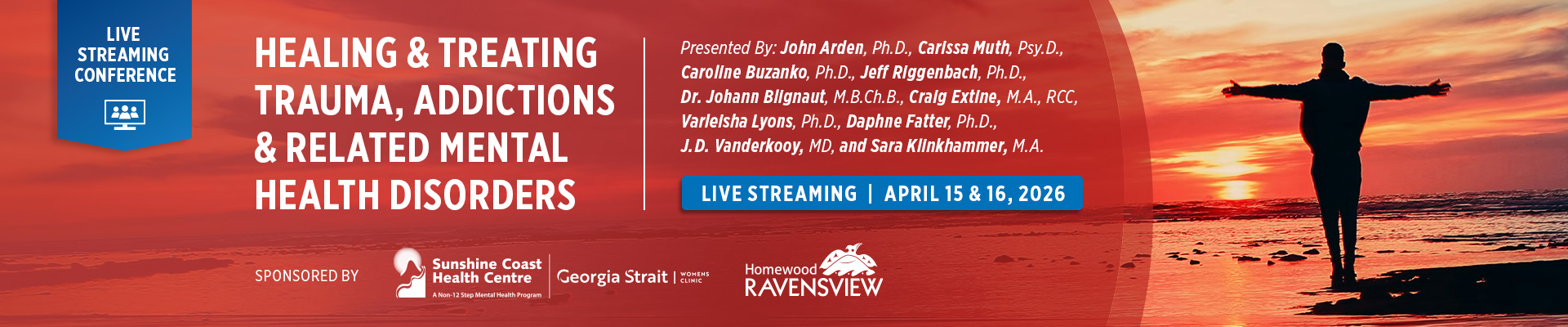
Join leading clinicians and researchers for a two-day virtual conference exploring evidence-informed, integrated approaches to trauma, addictions, and complex co-occurring mental health conditions. This conference brings together neuroscience, psychotherapy, medical perspectives, Indigenous healing frameworks, and skills-based interventions to support effective, individualized care.
This conference is designed for mental health professionals and allied health practitioners. Sessions emphasize practical tools, interdisciplinary collaboration, and contemporary clinical frameworks that move beyond rigid diagnostic models toward holistic healing and long-term recovery.
LIVE STREAM: April 15 – 16, 2026 from 8:30am – 4:00pm PST (Vancouver, BC) Please adjust your start time according to your specific time zone.
ON-DEMAND: Access Expires: May 25, 2026 – Recorded footage & course content certificate, videos, quiz. Please allow 3 – 5 business days for footage to be processed. Extensions cannot be granted under any circumstances.

April 16, 2026 | Day Two
Integrating Indigenous Healing Through Spiritual Traditions, Cultural Practices and Storytelling
Presented by Varleisha Lyons, Ph.D., OTD, OTR/L 
8:30am – 10:00am (90 minute session)
This session explores trauma through a holistic, culturally grounded lens, focusing on intergenerational trauma and its historical roots and ongoing effects on identity, culture, and well-being. Participants will examine the role of spirituality in healing, Indigenous ceremonial practices that foster resilience, and storytelling as a powerful vehicle for preserving culture and promoting healing across generations. The session encourages trauma-informed practice that honors cultural context, spiritual wisdom, and collective strength.
MID MORNING BREAK: 10:00AM – 10:15AM
 Traumatic Memories: Evidence-Based Approaches to Trauma Processing
Traumatic Memories: Evidence-Based Approaches to Trauma Processing
Presented by Daphne Fatter, Ph.D.
10:15am – 11:45am (90 minute session)
This presentation provides a clear framework for understanding traumatic memory and how it differs from non-traumatic memory. Dr. Fatter reviews evidence-based trauma-processing models and guides clinicians in making informed decisions about readiness, timing, and clinical indicators for trauma processing, emphasizing sound judgment and markers of therapeutic completion.
Lunch Break: 11:45AM – 12:30PM
Challenges in the Treatment of Eating Disorders
Presented by J.D. Vanderkooy, MD, BSc, FRCPC
12:30PM – 1:30PM (60 minute session)
This session addresses the multifactorial nature of eating disorders and the complex challenges involved in treatment. Topics include medical and pharmacological considerations related to malnutrition, co-occurring psychiatric disorders, interpersonal and family dynamics, resistance to treatment, and issues of identity and sense of self. Participants will gain insight into integrated approaches for providing comprehensive, responsive care.
Break: 1:30PM – 1:45PM
 Comparing Biomedical Versus Psychedelic Ketamine Treatments for Depression: The Importance of Connectedness
Comparing Biomedical Versus Psychedelic Ketamine Treatments for Depression: The Importance of Connectedness
Presented by Sara Klinkhamer, M.A.
1:45PM – 2:45PM (60 minute session)
This workshop examines ketamine treatment through both biomedical and psychedelic perspectives, exploring why ketamine can produce rapid antidepressant effects and why those effects may be short-lived when used alone. Framing depression as a form of disconnection, the session highlights ketamine-assisted psychotherapy (KAP) as an integrative model that combines medical, psychedelic, and relational elements, while encouraging ethical and critical consideration of ketamine’s off-label use in Canada and the U.S.
Break: 2:45PM – 3:00PM
 Advanced CBT Skills Training
Advanced CBT Skills Training
Presented by Jeff Riggenbach, Ph.D.
3:00PM – 4:00PM (60 minute session)
This one-hour workshop focuses on advanced, skills-based cognitive behavioural therapy (CBT) approaches for treating individuals with complex and co-occurring mental health conditions in inpatient settings. Drawing on neurobiological principles and evidence-informed CBT strategies, the session addresses common clinical challenges including impulsivity, emotional dysregulation, substance use, and treatment resistance. Participants will learn practical, adaptable interventions to enhance engagement, manage high-risk behaviours, and support stabilization and skill development within the structure and demands of inpatient care.